How to Spot & Treat a Root Canal Infection

Table of Contents
- What is a Root Canal Infection?
- Signs of a Root Canal Infection
- Will You Feel It Before You See It?
- What to Expect During a Root Canal
- Why Treat It Quickly?
- Root Canal FAQ
- References
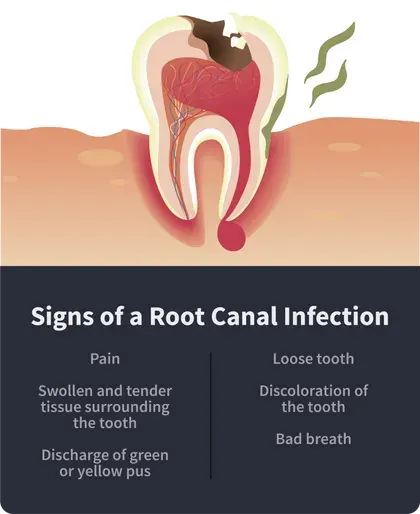
Signs of a root canal infection include pain, discharge, discoloration, swelling, and bad breath. A root canal infection is a serious issue that must be promptly addressed.
What is a Root Canal Infection?
When the tooth’s hard outer layer (the enamel) is worn down by decay, it leaves the softer inner layer (the pulp) vulnerable to bacterial infection. The pulp contains all the live elements of a tooth, like tissue, blood vessels, and nerve endings.
When it gets severely infected, it needs to be removed to prevent the spread of the infection through your bloodstream to other parts of your body. A root canal is a procedure in which infected pulp is removed, and the cavity is filled with a latex-based polymer filler, called gutta-percha.
In some instances, the bacterial infection persists after the procedure, and this is what we refer to as a root canal infection. It happens for a variety of reasons:
A narrow root canal is harder to clean and disinfect, and it may house bacteria.
Accessory canals can house bacteria and reinfect the tooth after the procedure.
If there is a delay in the placement of an artificial crown or permanent restoration, bacteria may get a chance to reinfect the tooth.
A crack or new cavity can instigate reinfection.
To spot it in time, you need to understand the warning signs and symptoms of a root canal infection.
How Do You Know if You Have a Root Canal Infection?
The most common signs of a root canal infection are pain, swelling, bad breath, discoloration and discharge.
Depending on the severity of the infection, pain caused by this kind of infection ranges from mild tenderness to a throbbing pain that lasts for hours and is essentially unbearable. This kind of pain is usually exacerbated by pressure (the weather) and temperature of food or liquids in your mouth (especially hot and cold beverages).
If the tissue surrounding the tooth is swollen and painful when you apply pressure, it’s a sign that the tooth may be infected. Tissues are often redder than the surrounding tissue and feels warm to the touch. In severe cases, the swelling may be visible on your face and neck.
Sometimes, the swollen tissue releases greenish or yellowish pus. This is a definite sign of infection and requires immediate attention from a dental professional.
Chances are if you are having discharge from your gums, your pain level is probably already off the charts.
If one of your primary (adult) teeth is loose for no apparent reason (no injury), there’s a strong likelihood that the tooth is infected or dying. You need to get this tooth looked at.
As the infection continues, the tooth may become discolored (yellow or dark brown), which is a sign that there is dead tissue in the root canal. Again, this is an indication of a major issue that needs to be addressed by a dentist as soon as possible.
Infected tissue has a bad smell, which can leave you with a bad taste in your mouth or bad breath, no matter how many times you brush your teeth.
Will You Feel an Infection Before You See It?
It’s certainly possible to feel a root canal infection before noticing it. It usually starts as a mild tenderness when you bite down too hard, or it may be a sharp, temporary pain when you drink something that’s too hot or cold.
It’s easy to ignore because the pain doesn’t last too long. But when it occurs along with other symptoms, it could be an early sign of root canal infection.
What to Expect During a Root Canal
Dentists recommend root canal retreatment as it is the only way to save the infected tooth.
First, your dentist will take an x-ray of the infected tooth to see how much necrotic (dead) tissue needs to be removed.
Before the procedure, you will receive local anesthesia to numb the affected area. Then, the dentist will place a protective shield around your mouth and gums.
Using a dental drill, they will penetrate through the enamel and pulp to access the root canal area. Then, they will clean out the necrotic tissue and all traces of the filler used previously. Once that is done, they will dry out the area.
The next step involves filling the cavity with amalgam or composite, a “bandage” of sorts that protects the cavity while the root canal heals from the infection.
When it’s completely healed, the dentist may resort to placing a permanent crown over the tooth to prevent future infections. It may require that they carve away more enamel.
The Importance of Treating Your Infection Quickly
A root canal infection is like any other bacterial infection and will spread to the surrounding tissue if left unchecked. It can infect the gums, the surrounding teeth, and even facial tissues, so once you detect it, time is of the essence.Keep in mind that the body is not equipped to deal with infections inside the teeth. A root canal infection won’t go away on its own and will likely persist and grow worse with time. The longer you wait, the more teeth it can potentially affect
Catching it early makes it possible for your orthodontist to curb the infection before it spreads to the surrounding tissue. The most serious issue that doctors worry about related to infections is the development of sepsis, which is a toxic response to an infection. Sepsis can kill you. In cases of severe root canal infection, the only feasible treatment may be extraction. In extreme cases, root canal infections will even spread into the bloodstream. However, if the condition is diagnosed within the first few hours or days of infection, it’s quite possible to save the tooth and use measures to prevent reinfection. Visit your dentist as soon as you spot any signs of root canal infection to maximize your recovery chances.
Treatment for a Root Canal Infection FAQ
Follow your dentist’s instructions in preparation for the procedure. If the dentist prescribes any medications before the appointment, like an antibiotic, take them as prescribed. Consider eating a hearty meal, as you may not be able to eat for a few hours after the root canal.
Depending on the type of anesthesia your dentist will be using, you may or may not be able to drive after the appointment, so you may need to plan an alternative way of getting home. Talk to your dentist about which anesthesia you’ll be receiving and how groggy you will be after your root canal.
After diagnosing the need for a root canal, most treatments can be completed in one visit lasting between 30 and 90 minutes. For those with complicated oral health issues or severe root canal infections, treatment may take more than one visit and require more time.
Your dentist will use some form of anesthesia to ensure the procedure isn’t painful at all. Usually, local anesthesia is used. In some cases, other options may be used, such as sedatives, nitrous oxide, or IV (intravenous) sedation.
After a root canal treatment, although you’re likely to feel some relief at the infection being removed, you may experience soreness or discomfort in the area during recovery. You may also have heightened tooth sensitivity for one to two weeks. Over-the-counter pain relievers could help these symptoms, or your dentist may prescribe something stronger.
Your pain or discomfort should only be mild to moderate. If you are experiencing more serious pain, or throbbing, you should call your dentist or seek medical attention right away. It may be a sign of root canal complications or of root canal failure.
It’s important to follow your dentist’s instructions after a root canal procedure. Your dentist may tell you not to eat or drink for a few hours after the procedure or at least until your anesthesia has worn off. They may also instruct you not to brush your teeth or floss immediately after the root canal.
When it’s okay for you to brush again, be sure to use a soft-bristled toothbrush and be gentle in the area of the root canal to avoid irritation that can impede the healing process.
Practicing good oral hygiene will also help your mouth recover after a root canal. A daily dental care routine that includes brushing twice a day, flossing daily, and using an antimicrobial mouthwash will help ensure the sensitive area will be kept clean and free of bacteria buildup.
Most root canals, especially those performed on single teeth or teeth near the front of the mouth, can be performed by your general dentist.
For complicated dental issues involving multiple teeth, or a tooth with various roots, you may be referred out to an endodontist — a dentist who is a specialist in treating root canals and diagnosing tooth pain.
About 98 percent of root canals are successful. Even with such a high success rate, there are people who experience a failed root canal or root canal complications that require emergency care.
The most common reason for a failed root canal is that it was performed on a tooth that was too damaged to successfully receive treatment.
While mild to moderate pain or sensitivity may be normal after a root canal, severe pain that affects your daily activities or feels as though it’s throbbing is not. If you are experiencing serious pain after your root canal, you should seek immediate medical care.
Other signs that you’re experiencing a failed root canal or root canal complications include swelling in the gums, pus, gum boils or blisters, sinus problems or headaches, or discolored teeth.
Tooth extraction is the only alternative when it comes to repairing a tooth that’s in need of a root canal. In some cases, a tooth may be too damaged to receive a successful root canal treatment and may need to be extracted.
If a tooth does need to be extracted, it’s important to consider treatment options to replace the lost tooth. A missing tooth can have a negative impact on oral health, potentially weakening the jawbone and causing bone loss and tooth decay. It can also affect quality of life by limiting eating and speech.
Options for tooth replacement include dental implants, bridges, and partial dentures.
